A Next-Generation Platform: What are Healios’
Universal Donor Cells (UDCs)?
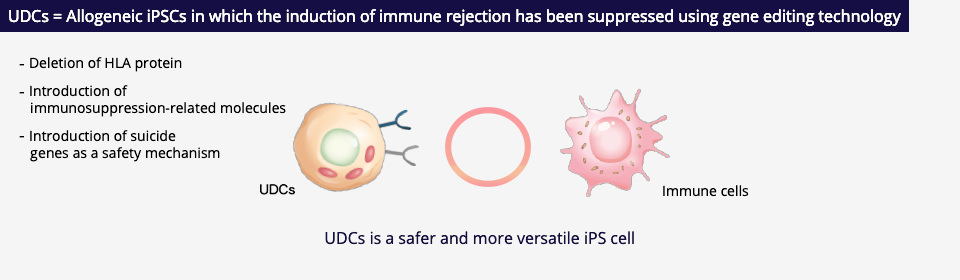
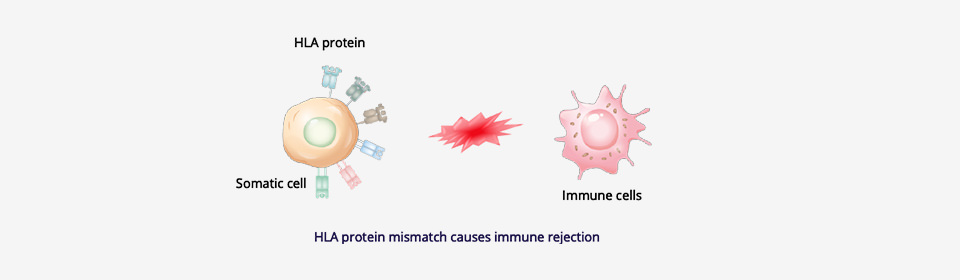
A universal donor cell is a kind of cell that can be used for transplantation into anyone. In other words, it is a cell in which the induction of immune rejection*1 (Human Leukocyte Antigen(HLA*2)mismatch) has been suppressed, and which can be used for patients requiring transplants without the need for the patient’s HLA to be matched.
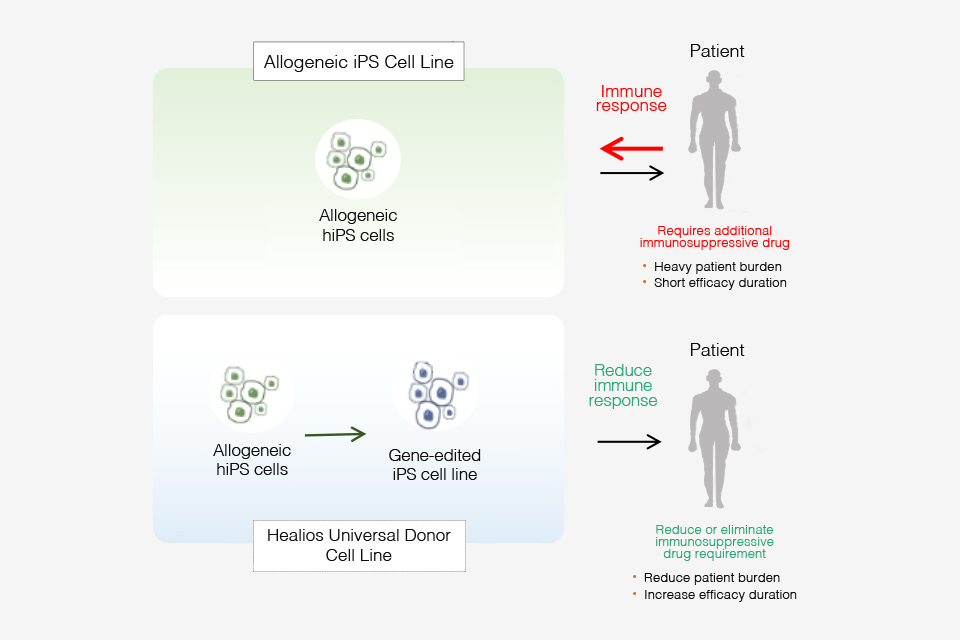
Healios has been conducting research and development that is focused on the potential of such universal donor cells, and we have successfully developed our company’s proprietary universal donor cells (the Healios “Universal Donor Cells” or “UDCs”) using iPS cells (induced pluripotent stem cells; “iPSCs”). Healios UDCs were developed from allogeneic iPSCs through the deletion of multiple HLA genes responsible for inducing immune rejection and the introduction of immunosuppression-related molecules, as well as the introduction of suicide genes*3 as a safety mechanism. These next-generation iPSCs can be used as a raw material in the development of regenerative medicine products as they retain both the inherent ability of iPSCs to renew themselves indefinitely and their pluripotency for differentiating into various kinds of cells, making them one of the important platform technologies (iPSC platform) of Healios.
- (Source)in-house data
Healios’ goal for the utilization of UDCs
As our UDCs retain the inherent ability of iPSCs to renew themselves indefinitely and their pluripotency for differentiating into various kinds of cells, they can be used to generate various kinds of target cells and tissues. The target cells and tissues generated from UDCs serve as regenerative medicine products that can be utilized for cell therapy and replacement therapy (the replacement of damaged cells and tissues in patients).
Healios aims to utilize UDCs for applications in next-generation immune-oncology, ophthalmology, and organ buds. We are engaged in both the in-house development of regenerative medicine products as well as collaborations with other companies and research institutions regarding the R&D of novel therapeutic agents using UDCs.
Advantages of UDCs
Using cells and tissues generated with UDCs can alleviate the stress on the patient’s body after transplantation. Presently, there are two ways to generate cells and tissues from iPSCs: by using the patient’s own cells (autologous cells) or the cells of a donor (allogeneic cells).
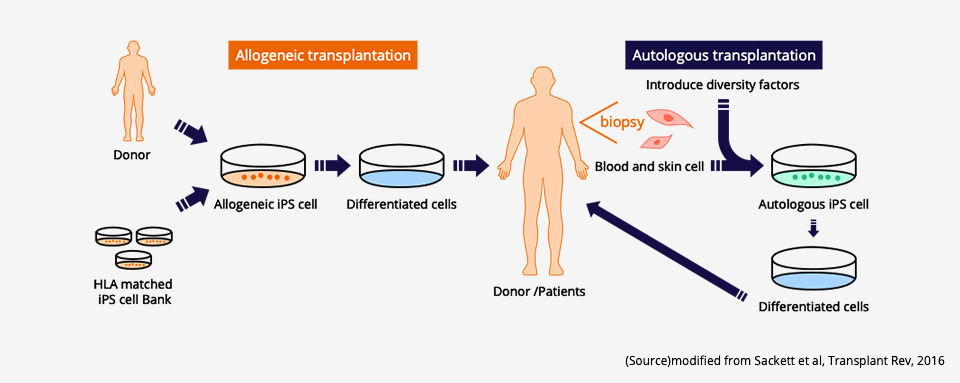
There is no immune rejection in the case of autologous transplantation since the patient uses their own cells, which allows the transplanted cells and tissues to develop in their body without any issues. While autologous transplantation results in lower stress on the patient’s body, this method is time-consuming and costly as the cells and tissues for autologous transplantation need to be generated to suit each unique individual.
On the other hand, while the generation of cells and tissues needed for allogeneic transplantation from in-stock iPSCs derived from donors requires less time and is less expensive than in the case of autologous transplantation, immune rejection that results in graft failure of the transplanted cells and tissues will occur if there is a mismatch with the patient’s immunophenotype. To prevent this rejection from occurring, immunosuppressive drugs must be administered for a long period of time, which places additional stress on the patient’s body.
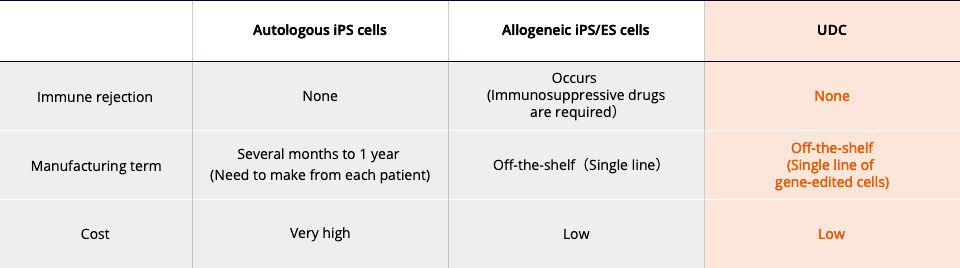
UDCs are a kind of allogeneic iPSC that has been genetically edited to prevent immune rejection. Cells and tissues generated from UDCs have a lower risk of inducing immune rejection after transplantation and a higher graft success rate in the patient’s body. The use of UDCs is expected to lead to forms of treatment that can shorten the time needed to generate the required cells and tissues, reduce the need for immunosuppressive drugs after transplantation, and alleviate the stress on the patient’s body.
*1 Immune rejection
When the cells or organ (graft) of a donor whose HLA type does not match the patient’s or whose HLA gene is defective is transplanted, the graft is regarded as foreign and will be attacked and destroyed by the immune cells of the host (patient).
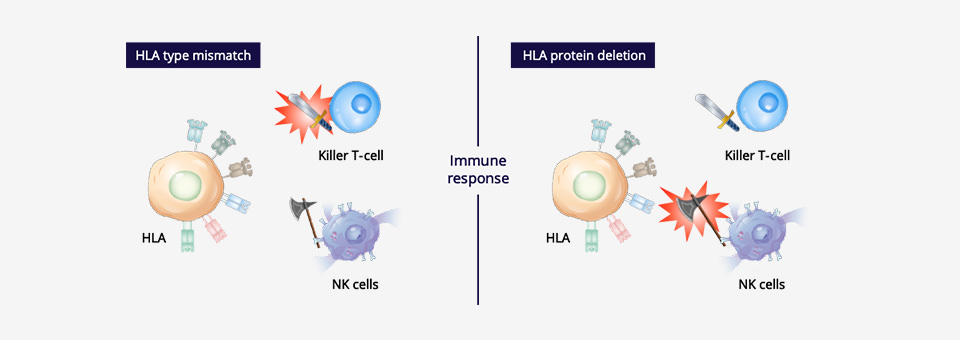
*2 HLA
HLA (Human Leukocyte Antigen) is a group of important protein molecules expressed in many human cells which serve to identify cells that belong to the individual. HLA is considered the blood type of leukocytes and is widely distributed across almost all of the cells and fluids in the body. There are several kinds of HLA, and the possible combinations of HLA are innumerable and tremendously diverse. Anything in the body with an HLA type that differs from the individual’s HLA type is identified as foreign and will be rejected and attacked by their immune response.
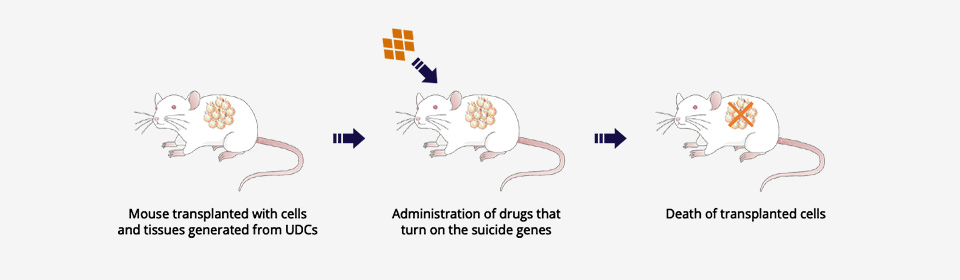
*3 Suicide genes
Suicide genes are artificial genes that can manually induce the death of the cell itself. These genes serve as a safety mechanism where cells that cause abnormalities can be eliminated by activating the suicide gene and inducing cell death.